Congestive Heart Failure (CHF) affects millions of Americans, causing significant health complications and decreased quality of life. This condition develops when the heart muscle cannot pump blood efficiently enough to meet the body’s needs. Understanding the root causes of CHF is essential for both prevention and effective management.
Various factors contribute to the development of CHF, ranging from lifestyle choices to underlying medical conditions. Coronary artery disease, high blood pressure, and previous heart attacks are among the leading causes, while diabetes, obesity, and certain medications can also increase risk.
At RGV Direct Care, we recognize that early identification of these risk factors through comprehensive primary care services is crucial for preventing CHF progression and improving patient outcomes.
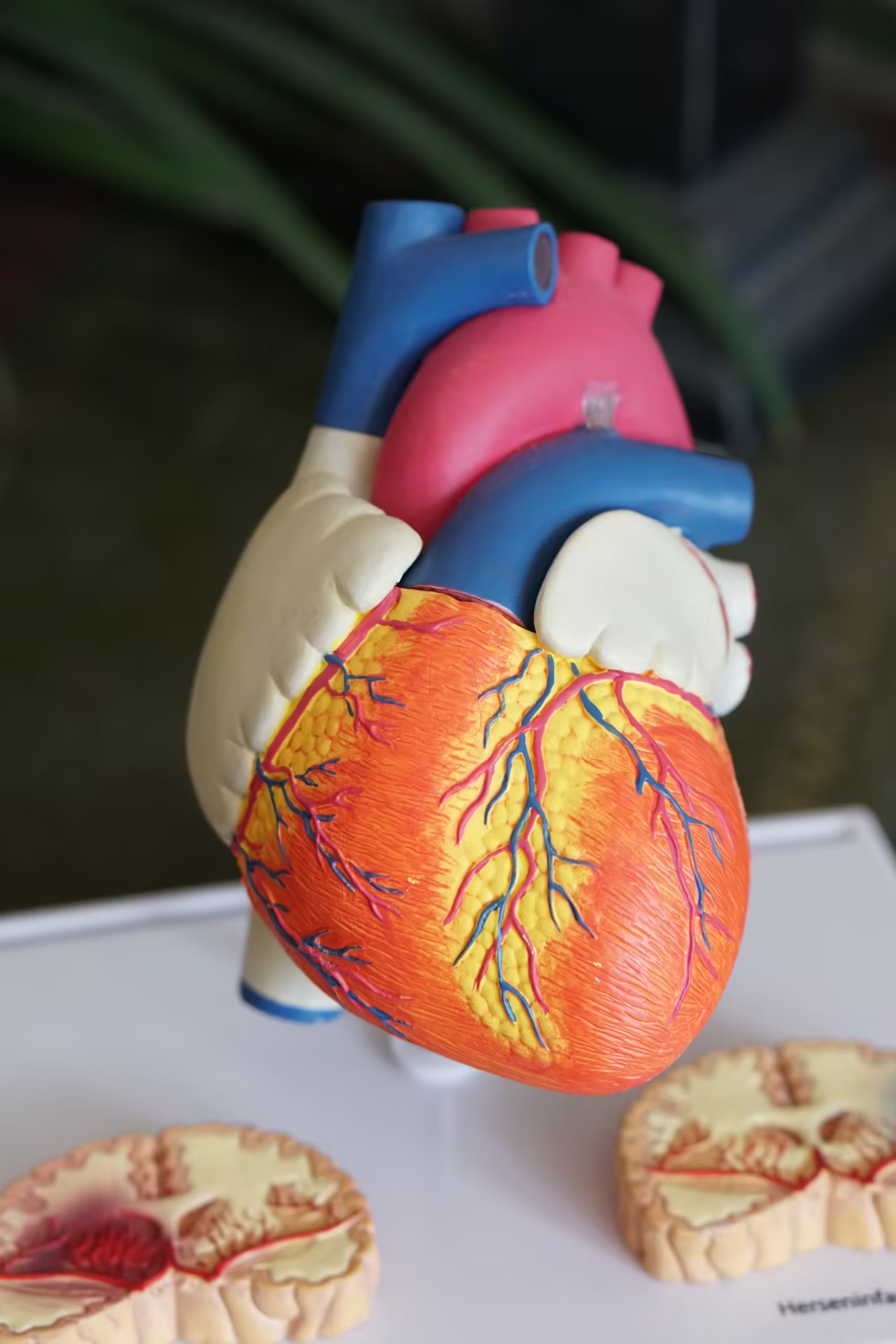
Exploring Congestive Heart Failure (CHF)
Congestive Heart Failure (CHF) occurs when the heart muscle can’t pump blood effectively, causing fluid buildup in the lungs, liver, and other body tissues. It’s a progressive condition affecting 6.2 million Americans, significantly impacting quality of life and increasing mortality risk.
What Exactly Is CHF?
CHF develops when the heart’s pumping ability weakens, preventing adequate blood circulation throughout the body. This leads to fluid retention in various tissues, particularly the lungs, causing congestion—hence the term “congestive” heart failure.
The heart compensates initially through mechanisms like:
- Enlargement of heart chambers
- Increased muscle mass
- Faster heart rate
- Narrowing of blood vessels
These compensatory changes maintain cardiac output temporarily but eventually fail, worsening symptoms and organ function.
Types of Heart Failure
Heart failure manifests in several forms based on which part of the heart is affected:
Left-Sided Heart Failure
- Reduced Ejection Fraction (HFrEF): The heart muscle can’t contract effectively, reducing the amount of blood pumped out.
- Preserved Ejection Fraction (HFpEF): The heart muscle becomes stiff and can’t relax properly between beats.
Right-Sided Heart Failure
Typically occurs as a result of left-sided failure, causing fluid retention in the abdomen, legs, and feet.
Biventricular Failure
Affects both sides of the heart simultaneously, often indicating advanced disease.
Common Symptoms
CHF symptoms vary depending on the type and severity but commonly include:
- Shortness of breath during activity or when lying down
- Persistent coughing or wheezing
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Reduced exercise capacity
- Sudden weight gain from fluid retention
- Difficulty concentrating or decreased alertness
Early recognition of these symptoms is crucial for timely intervention.
Diagnostic Approach
Diagnosing CHF involves multiple assessments:
- Comprehensive medical history review
- Physical examination focusing on heart sounds and fluid retention signs
- Blood tests including BNP (B-type natriuretic peptide)
- Chest X-rays to check for heart enlargement and lung congestion
- Electrocardiogram (ECG) to detect abnormal heart rhythms
- Echocardiogram to measure ejection fraction and heart function
- Stress tests to evaluate heart performance during physical activity

Common Causes of CHF
Congestive Heart Failure (CHF) develops from various underlying conditions that damage or weaken the heart muscle over time. Understanding these primary causes helps in prevention strategies and early intervention, which can significantly improve outcomes for patients.
Coronary Artery Disease
Coronary artery disease (CAD) stands as the leading cause of CHF in the United States, accounting for about 70% of heart failure cases. CAD occurs when cholesterol-containing deposits (plaques) build up in the coronary arteries, restricting blood flow to the heart muscle. This reduced blood flow damages heart tissue, weakening its pumping ability and eventually leading to heart failure. Risk factors for CAD include smoking, high cholesterol levels, diabetes, and family history of heart disease. Regular cardiac assessments can identify early signs of coronary artery disease before it progresses to CHF.
High Blood Pressure
Hypertension places excessive strain on the heart by forcing it to work harder to pump blood against increased resistance in the arteries. This constant additional workload causes the heart muscle to thicken and become stiffer, a condition called left ventricular hypertrophy. Over time, the overworked heart muscle weakens and loses elasticity, diminishing its ability to fill and pump efficiently.
Cardiomyopathy
Cardiomyopathy refers to diseases affecting the heart muscle itself, making it harder for the heart to pump blood effectively. Three main types contribute to CHF: dilated cardiomyopathy (enlarged heart chambers), hypertrophic cardiomyopathy (thickened heart walls), and restrictive cardiomyopathy (stiffened heart tissue). Causes of cardiomyopathy include genetic factors, viral infections, alcohol abuse, certain medications, and autoimmune disorders. In some cases, the exact cause remains unknown (idiopathic cardiomyopathy). Early detection through cardiac imaging techniques like echocardiograms helps manage the condition before it progresses to severe heart failure.
Heart Valve Disorders
Heart valve problems develop when the valves that regulate blood flow through the heart chambers don’t function properly. Two common valve disorders leading to CHF include stenosis (narrowing of valves) and regurgitation (leaking valves). When heart valves don’t open or close correctly, the heart must work harder to maintain proper circulation, eventually leading to heart muscle weakening and failure. Heart valve disorders may result from congenital abnormalities, infections like endocarditis, rheumatic fever, or age-related degenerative changes. Regular cardiac check-ups with auscultation can detect valve abnormalities through heart murmurs, allowing for earlier intervention and potentially preventing progression to CHF.
Lifestyle Factors Contributing to CHF
Lifestyle choices significantly impact heart health and can increase the risk of developing Congestive Heart Failure (CHF). Daily habits related to diet, physical activity, and substance use create cumulative effects on cardiovascular function that may lead to heart damage over time. Recognizing and modifying these lifestyle factors offers an opportunity to prevent CHF development or slow its progression.

Poor Diet and Obesity
Poor dietary habits directly contribute to CHF development through multiple physiological pathways. Diets high in sodium (exceeding 2,300mg daily) increase fluid retention and blood pressure, forcing the heart to work harder with each beat. Excessive consumption of processed foods, saturated fats, and refined sugars leads to atherosclerosis, insulin resistance, and metabolic dysfunction—all precursors to heart failure.
Obesity, affecting 42.4% of American adults, places extraordinary strain on the cardiovascular system. Each additional pound of fat tissue requires approximately one mile of new blood vessels for adequate perfusion, significantly increasing cardiac workload. Research published in the Journal of the American College of Cardiology shows that individuals with obesity have a 60-90% higher risk of developing heart failure compared to those with normal weight. The metabolic changes associated with excess weight—including elevated inflammatory markers, insulin resistance, and altered lipid profiles—create a perfect storm for myocardial damage.
Lack of Exercise
Physical inactivity represents a major modifiable risk factor for CHF development. Regular exercise strengthens the heart muscle, improves circulation, and enhances the body’s oxygen utilization efficiency. The American Heart Association reports that sedentary individuals face a 35% higher risk of developing heart failure compared to physically active counterparts.
Cardiovascular deconditioning from prolonged inactivity leads to:
- Reduced cardiac output capacity
- Decreased vascular elasticity
- Impaired mitochondrial function in heart cells
- Higher resting heart rates placing additional strain on cardiac tissue
Even modest physical activity provides protective benefits. Studies show that walking 30 minutes five days weekly reduces CHF risk by approximately 25%, demonstrating the critical importance of incorporating regular movement into daily routines.
Smoking and Alcohol Consumption
Tobacco use damages the cardiovascular system through multiple mechanisms, making it a significant CHF risk factor. Cigarette smoke contains over 7,000 chemicals that harm blood vessels, increase blood pressure, and reduce oxygen delivery to tissues. Carbon monoxide from smoke binds to hemoglobin 240 times more readily than oxygen, severely compromising the heart’s oxygen supply. Smokers experience twice the risk of developing heart failure compared to non-smokers, with risk remaining elevated for up to 15 years after quitting.
Excessive alcohol consumption contributes to cardiomyopathy and heart failure through direct toxic effects on heart muscle cells. While moderate drinking (one daily drink for women, two for men) may be safe for most people, chronic heavy consumption leads to:
- Weakened heart muscle (alcoholic cardiomyopathy)
- Disrupted heart rhythm
- Elevated blood pressure
- Compromised nutrient absorption affecting cardiac function
Medical Conditions That Increase CHF Risk
Several pre-existing medical conditions significantly elevate the risk of developing congestive heart failure. These conditions often damage the heart over time or place additional stress on the cardiovascular system, eventually compromising heart function and leading to CHF.
Diabetes
Diabetes substantially increases the risk of developing congestive heart failure, with diabetic patients facing 2-5 times higher risk than non-diabetics. This chronic metabolic disorder damages blood vessels and nerves through prolonged high blood sugar levels, directly affecting heart function. The damage to blood vessels accelerates atherosclerosis, restricting blood flow to the heart muscle and potentially causing heart muscle damage. Additionally, diabetes often promotes insulin resistance, which forces the heart to work harder and can lead to cardiac hypertrophy.
Diabetic cardiomyopathy, a specific heart muscle disorder in people with diabetes, occurs even without coronary artery disease or hypertension. Managing diabetes through medication adherence, regular blood sugar monitoring, and lifestyle modifications is crucial for reducing CHF risk in diabetic patients.
Sleep Apnea
Sleep apnea creates a significant pathway to heart failure through multiple physiological mechanisms. This sleep disorder, characterized by repeated breathing interruptions during sleep, affects an estimated 25 million Americans. Each breathing pause triggers a stress response, releasing hormones that increase blood pressure and heart rate. Over time, this repetitive strain weakens the heart muscle and disrupts its normal electrical patterns.
Sleep apnea also causes chronic oxygen deprivation, forcing the heart to pump harder to compensate for reduced oxygen levels. This leads to right-sided heart failure in many cases. The condition is particularly dangerous because:
- It raises blood pressure during both sleep and waking hours
- It elevates inflammation markers throughout the body
- It increases carbon dioxide retention, further stressing the cardiovascular system
- It disrupts normal heart rhythm, with 40% of sleep apnea patients developing arrhythmias
Kidney Disease
Kidney disease and heart failure share a dangerous bidirectional relationship that creates a cycle of worsening health outcomes. Chronic kidney disease (CKD) affects approximately 37 million Americans and dramatically increases CHF risk through several mechanisms. The kidneys’ reduced ability to filter waste leads to fluid retention, directly increasing strain on the heart. This excess fluid forces the heart to pump harder, eventually leading to cardiac enlargement and dysfunction.
Kidney disease also disrupts the body’s delicate electrolyte balance, particularly potassium and sodium levels, which can trigger dangerous heart rhythm abnormalities. The condition frequently causes anemia, reducing oxygen delivery to tissues and forcing the heart to compensate through increased output. CKD additionally contributes to systemic inflammation, accelerating blood vessel damage and heart muscle deterioration.
Patients with both conditions experience dramatically higher mortality rates, with 5-year survival rates dropping to approximately 20% when both conditions are present. Protecting kidney function through blood pressure management, medication adherence, and limiting nephrotoxic substances is essential for CHF prevention in at-risk individuals.
Comprehensive Approach at RGV Direct Care
At RGV Direct Care, CHF treatment plans integrate pharmaceutical interventions, procedural options, and lifestyle modifications tailored to each patient’s specific underlying causes. Our approach includes:
- Coordination with cardiac specialists for advanced interventional procedures
- Monitoring systems detecting early signs of CHF exacerbation
- Patient education emphasizing self-care strategies specific to underlying conditions
This multimodal treatment strategy results in reduced hospitalizations, improved quality of life, and enhanced long-term prognosis for patients with various forms of congestive heart failure.
Conclusion
Understanding the causes of CHF is crucial for effective prevention and management of this serious condition. From coronary artery disease and hypertension to lifestyle factors like poor diet and lack of exercise each risk factor represents an opportunity for intervention.
Early recognition of warning signs coupled with regular screenings can significantly improve outcomes. Patients with pre-existing conditions such as diabetes kidney disease and sleep apnea need particularly vigilant monitoring.
The good news is that many CHF risk factors are modifiable. Implementing heart-healthy lifestyle changes maintaining proper medication adherence and working closely with healthcare providers can help prevent or slow CHF progression. With comprehensive care and proactive management patients can maintain better cardiovascular health and quality of life.
Frequently Asked Questions
What is Congestive Heart Failure (CHF)?
Congestive Heart Failure is a condition where the heart cannot pump blood effectively, causing fluid buildup in the lungs, liver, and other body tissues. It affects approximately 6.2 million Americans and leads to reduced quality of life and increased mortality risk. CHF is progressive but can be managed with proper medical care and lifestyle changes.
What are the main causes of Congestive Heart Failure?
The leading cause of CHF is coronary artery disease (about 70% of cases), followed by high blood pressure, cardiomyopathy (heart muscle disease), and heart valve disorders. Medical conditions like diabetes, kidney disease, and sleep apnea significantly increase risk. Lifestyle factors including poor diet, obesity, lack of exercise, smoking, and excessive alcohol consumption also contribute substantially.
What are the symptoms of Congestive Heart Failure?
Common symptoms include shortness of breath (especially during activity or while lying down), persistent coughing or wheezing, fatigue and weakness, swelling in the legs, ankles, and feet, rapid or irregular heartbeat, reduced ability to exercise, and sudden weight gain from fluid retention. Early recognition of these symptoms is crucial for timely intervention.
How is Congestive Heart Failure diagnosed?
Diagnosis involves a comprehensive approach including medical history review, physical examination, blood tests, chest X-rays, electrocardiograms (ECG), echocardiograms, and stress tests. Doctors may also measure ejection fraction to determine heart pumping efficiency and classify the type of heart failure.
Can Congestive Heart Failure be prevented?
Yes, CHF can often be prevented by managing risk factors through lifestyle modifications. This includes maintaining a heart-healthy diet low in sodium, regular exercise, weight management, avoiding smoking and excessive alcohol, controlling blood pressure and cholesterol, and properly managing conditions like diabetes. Regular health screenings are also essential for early intervention.
What is the difference between left-sided and right-sided heart failure?
Left-sided heart failure occurs when the left ventricle can’t effectively pump blood to the body, causing fluid buildup in the lungs. It can be further classified as reduced or preserved ejection fraction. Right-sided heart failure happens when the right ventricle can’t pump blood to the lungs properly, causing fluid retention in the abdomen and lower extremities. Many patients develop biventricular failure affecting both sides.
How does obesity contribute to heart failure?
Obesity places extraordinary strain on the cardiovascular system by increasing blood volume, raising blood pressure, and causing metabolic dysfunction. It increases heart failure risk by 60-90%. Excess fat tissue requires additional blood vessels, forcing the heart to work harder. Obesity also contributes to inflammation, insulin resistance, and increased risk of other conditions that damage the heart.
What role does diabetes play in developing CHF?
Diabetic patients face 2-5 times higher risk of developing heart failure. Prolonged high blood sugar damages blood vessels and nerves that control the heart. Diabetes accelerates atherosclerosis (artery hardening), causes metabolic abnormalities affecting heart muscle function, and often co-occurs with other risk factors like obesity and hypertension. Proper diabetes management significantly reduces CHF risk.
How does sleep apnea affect heart health?
Sleep apnea causes repeated breathing interruptions during sleep, leading to oxygen deprivation that stresses the cardiovascular system. This triggers increased blood pressure, irregular heart rhythms, and increased inflammation. Over time, the heart becomes strained from working harder to compensate for reduced oxygen, potentially leading to heart failure. Treating sleep apnea can significantly improve heart function.
What treatments are available for CHF?
Treatment depends on the underlying cause but generally includes medications (ACE inhibitors, beta-blockers, diuretics), lifestyle modifications, and sometimes devices or surgery. For coronary artery disease, treatments may include angioplasty or bypass surgery. Valve disease might require repair or replacement. Comprehensive approaches include medication management, procedural interventions, and addressing contributing conditions like diabetes or sleep apnea.
What lifestyle changes help manage CHF?
Effective lifestyle modifications include following a low-sodium diet (under 2,000mg daily), regular moderate exercise as tolerated, weight management, avoiding tobacco and limiting alcohol, monitoring fluid intake, managing stress, and getting adequate rest. Self-monitoring daily weight and symptoms is crucial. These changes complement medical treatment and can significantly improve quality of life.
How important is medication adherence for CHF patients?
Medication adherence is critical for CHF management. Properly taking prescribed medications helps control symptoms, slow disease progression, reduce hospitalizations, and improve survival rates. Missing doses can lead to rapid symptom worsening and complications. Patients should maintain open communication with healthcare providers about any side effects or concerns to ensure optimal medication management.